OB - Exercise in pregnancy
Benefits of Exercise in Pregnancy

- Vaginal delivery

Lower incidence of:
- Excessive gestational weight gain
- Gestational diabetes mellitus
- Gestational hypertensive disorders*
- Preterm birth
- Cesarean birth
- Lower birth weight
Modified from Berghella V, Saccone G. Exercise in pregnancy! Am J Obstet Gynecol 2017;216:335–7.
GYN- Introduction to Long Lasting Reversible Contraception
The IUD is a small, T-shaped, plastic device that is inserted into and left inside the uterus. There are two types of IUDs:
- The hormonal IUD releases the hormone progestin into the uterus. There are different brands of hormonal IUDs that last for different lengths of time. Depending on the brand, they are approved for up to 3 to 7 years of use.
- The copper IUD releases copper into the uterus. This IUD does not contain hormones. It is approved for up to 10 years of use.
The copper in the copper IUD interferes with sperm’s ability to move. When sperm stop acting normally, it is harder for them to enter the uterus and reach an egg.
The IUD has the following benefits:
- It is easy to use. Once it is in place, you do not have to do anything else to prevent pregnancy. It is effective for years.
- No one can tell that you are using birth control.
- It does not interfere with sex or daily activities. You can use a tampon with it.
- It can be inserted immediately after an abortion, a miscarriage, or childbirth. It can be used while breastfeeding.
- Almost all women are able to use an IUD. There are few medical problems that prevent its use.
- If you want to get pregnant or if you want to stop using it, you can have the IUD removed. You can start trying to get pregnant right after removal. Using an IUD does not affect your ability to get pregnant in the future.
- Over time, the hormonal IUDs help decrease menstrual pain and heavy menstrual bleeding.
- The copper IUD also is the most effective form of emergency contraception (EC). When used for EC, it should be placed in the uterus within 5 days (120 hours) of having unprotected sex. Then you can leave it in and use it as a regular form of birth control. (Read Emergency Contraception to learn more.)
You may have a pregnancy test before the IUD is placed. If you are at risk of STIs, you may need STI tests either before placement or on the day of insertion.
The IUD has strings made of thin plastic threads. Your health care professional will use the strings to remove the IUD when you decide to stop using it. After placement, the strings are trimmed so that they extend just past the cervix into your vagina.
The strings should not bother you, but in rare cases your sexual partner may feel them during sex. If this happens and it is a concern, your health care professional may be able to trim the strings.
The copper IUD protects against pregnancy right away and you do not have to use a backup method or avoid intercourse.
When a woman uses an IUD, changes in menstrual bleeding are normal and not harmful. Some changes can be temporary and may go away as your body gets used to the IUD. Others may last for as long as you have the IUD. If you have changes in bleeding that concern you, talk with your health care professional. Often, medications can help with some of the bleeding changes that happen with IUDs.
With the copper IUD, painful periods and bleeding may increase during the first months of use. Over-the-counter pain relievers may be used for pain and bleeding.
Hormonal IUDs may cause frequent spotting, more days of bleeding, and heavier bleeding in the first months of use. Over time, the amount of menstrual bleeding and the length of your menstrual period usually decrease. Menstrual pain also usually decreases. For some women using a hormonal IUD, menstrual bleeding stops completely.
Some women also may experience other side effects, including
- headaches
- nausea
- breast tenderness
- mood changes
Serious complications from IUDs are rare. But some women do have problems. These problems usually happen during or soon after insertion:
- In a small number of women, the IUD may come out of the uterus. The entire IUD may come out, or only part of it may come out. The risk is higher in teenagers, women with heavy menstrual bleeding, and women who have an IUD inserted immediately after childbirth. If the IUD comes out, it is no longer effective. You may be able to have a new IUD placed.
- The IUD can go through the wall of the uterus during placement. This usually does not cause any major health problems, but the IUD will need to be removed. This is rare and happens in only about 1 out of every 1,000 placements.
- Pelvic inflammatory disease (PID) after IUD insertion happens very rarely. Using an IUD does not by itself increase the risk of PID. Women with an undiagnosed STI at the time of IUD insertion are more likely to develop PID than women without an STI. If you are at risk of STIs, you may be screened before you get an IUD.
- Rarely, pregnancy may occur while a woman is using an IUD. If pregnancy happens, and you wish to continue the pregnancy, the IUD should be removed if your health care professional can see the IUD in the cervix or if the strings are visible. If the IUD remains in place during pregnancy, there are increased risks of miscarriage and infection.
- In the rare case that a pregnancy happens with the IUD in place, there is a higher chance that it will be an ectopic pregnancy. This is a serious condition that needs medical attention right away.
The following symptoms may be a sign of a problem with your IUD. A health care professional should remove the IUD. Call your health care professional if you have any of the following:
- Severe pelvic pain
- Unexplained fever
- Unusual vaginal discharge
- Feeling the IUD in the cervix or vagina
- Signs of pregnancy: positive home pregnancy test, missed menstrual period, or other signs of pregnancy in addition to a missed period, such as nausea or breast tenderness
Citation: ACOG.org
Myosure Device
3 Simple Steps to Freedom From Polyps and Fibroids
Step 1
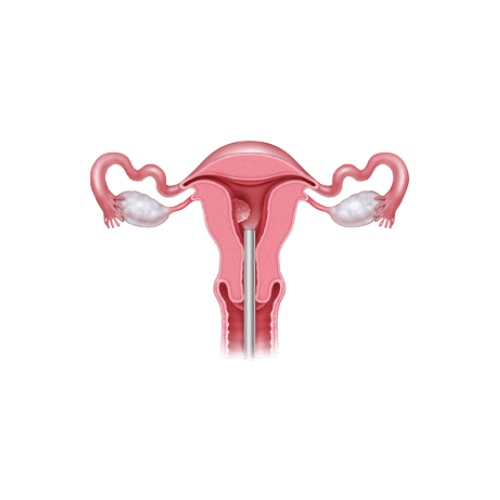
Your doctor opens your cervix (the opening to the uterus) slightly by passing through the body’s natural openings (i.e., through the vagina) and inserts a slender camera through your cervix and into your uterus, allowing him or her to see inside.
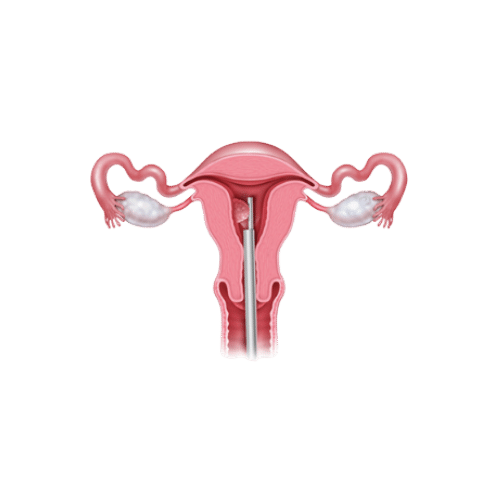
Your doctor passes a slender wand through your vagina into your uterus. The side of the wand gently cuts the fibroid or polyp into tiny pieces and suctions the removed tissue through a small open window into the wand and out of your body.
Step 2
Once the fibroid or polyp has been taken away, the wand is removed from the uterus. Nothing from the MyoSure tissue removal system is left in your body after the procedure.
Step 3
Citation: https://gynsurgicalsolutions.com/